Dear Reader,
Three Western New York counties reported an increase in overdose deaths since the pandemic. The Erie County Medical Examiner’s Office saw about one suspected overdose each day in March. While the deaths are suspected to be due to fentanyl, they can’t be confirmed as opioid-related overdoses until toxicology tests are complete.
For anyone currently struggling, the state’s Good Samaritan Law protects people who are trying to help someone in the midst of an overdose. Below the New York State Office of Addiction Services and Supports highlights the signs of opioid overdose.
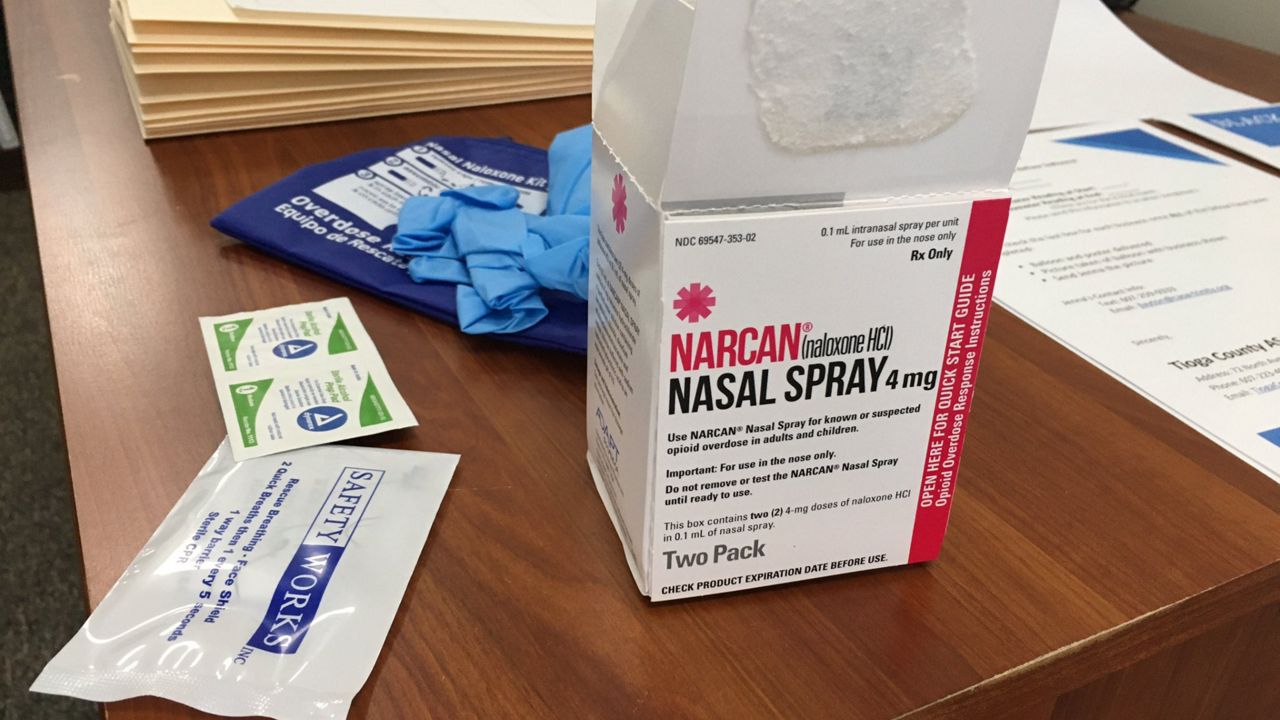
Roger Crystal, CEO of Opiant Pharmaceuticals and the lead inventor of the Narcan nasal spray, sat down to discuss how the pandemic is changing how communities address overdoses. Below are four takeaways from that interview.
The Q & A has been edited for clarity.
If you have any information about substance use treatment in New York or are in recovery and would like to share your story, please email me at Camalot.Todd@Charter.com.
Spectrum News Buffalo will be resuming #IAm1in5 Facebook Lives at 1 p.m. est, Thursday, May 7 with Heidi Billittier, the director of older adult services for Compeer of Greater Buffalo.
—Camalot K. Todd
Spectrum News: Tell me a little bit about how this pandemic has impacted opioid treatment for people who are in need of it.
Roger Crystal: Well, [let's] think about the situation in general, to give some perspective on how it then might be impacted by COVID-19. So I think the first consideration is how the crisis, which is described as an opioid crisis, has really become one of the fentanyl crisis. And that's based on data that shows almost 50,000 opioid overdose deaths (the most recent data we have is in 2018) over 60 percent, about 66 percent of those deaths contained fentanyl.
The issue around fentanyl is that it can infiltrate into other as drugs as well, other illicit substances. So what we see is that there's a lot more overdose deaths from cocaine, from methamphetamine and it appears that even fentanyl is getting into these substances so people aren't aware of whether overdosing on.
Spectrum News: Where these overdoses are taking place is moving away from places where there's a bystander who could administer Narcan or drugs that could potentially save this person from overdosing to a more private location.
How is the system changing to address this?
Roger Crystal: I'm not aware directly yet that the system is putting things in place to better respond to an opioid overdose within the context of COVID-19, unfortunately. The issue isn't an overdose, it's that it's an emergency that happens so fast that you can't really anticipate that well, when it happens and intervene.
What has to happen is having a commitment that our existing infrastructure, so predominantly first responder organizations, is still fully informed and empowered to address opioid overdose.
There are additional things we could potentially do.
It's interesting, and maybe our hope is that if we get much better at surveillance around COVID-19 and contact tracing around COVID-19, where there's potential outbreaks, if there's a huge investment in this — which I hope there is — they could be then be deploying that same technology and that same approach for fentanyl outbreaks because there are some parallels where we see unfortunately, we see in the news since COVID-19, some real spikes, multiple fentanyl overdose.
Spectrum News: Fentanyl is now being cut with different drugs so that the user may not actually know what they're taking. How can medical professionals and first responders address that?
Roger Crystal: That's a huge challenge and it's something that we're also trying to take on as a company.
The issue is can you detect fentanyl in a substance anyway? And there are kits out there, but the issue is that fentanyl can be very easily changed into other derivatives. So you might have heard of carfentanil. So a kit that detects fentanyl won't necessarily detect carfentanil.
So all of these derivatives of fentanyl ultimately are going to end up contaminating other drugs anyway. So there are efforts to try and address that — better detection and almost a better awareness of where the illicit drugs are coming from — and then can you somehow intersect upstream and really understand and take aggressive action against it. That's what we've been trying to do for quite a while as a country because all these other substances are illegal as well.
So the issue becomes if someone says overdose on fentanyl, can we do as much as possible to save that life with a reversal agent?
The issue of the moment is that while naloxone, and Narcan nasal spray in particular, has been a terrific way of curbing this opioid crisis and opioid overdose deaths would be far higher if we didn't have the issues around the naloxone we see that more and more naloxone is required to initially revive someone from fentanyl overdose.
And the other issue is that once you revive someone — if you're successful in doing so — the naloxone essentially wears off quicker than fentanyl wears off....they fall back into an overdose once again, which is particularly problematic if they choose not to go to the ER and get more definitive medical care.
Spectrum News: Tell me a little bit about co-prescribing and how that can be helpful for people who are at risk and are currently isolating because of the pandemic. While New York currently doesn’t have a co-prescribing law on books, there are several bills in the legislation process tackling this that passed the state Senate in February.
Roger Crystal: For people, who sometimes legally considered high risk of opioid overdose, but we recognize either requiring opioids either in the form of an opioid painkillers, they're in any pain treatment, or because perhaps they're taking methadone or buprenorphine and still might potentially be exposed to overdose because of that, that having access to an opioid overdose reversal agent might help save their life.
While overdose deaths may be on the rise, there are resources available.
For more of our coverage on mental health amid the COVID-19 pandemic click on the links below:
Stopping Misinformation From Spreading Amid the COVID-19 Pandemic
WNY Chapter of Alzheimer’s Association Offers Free Resources Amid COVID-19 Pandemic
Local Mental Wellness Resource Guide Helps Connect WNY Amid COVID-19
Addiction, Substance Use Help in WNY Amid the COVID-19 Pandemic
Coronavirus Changing Telehealth for Behavioral, Mental Health in New York
BryLin Uses Video, Telehealth To Help Children in Need of Mental Health Care Amid COVID-19
Hochul Talks With Advocates To Address Mental Health Care for Students
New York Emotional Hotline for Everyone, Buffalo Clergy Included
New York Continues To Battle the Opioid Epidemic During the Coronavirus Pandemic
Mental Health Advocates of WNY Help Children Navigate Coronavirus Pandemic