CHARLOTTE, N.C. — Roughly three years ago this month, North Carolina was dealing with its first few confirmed cases of COVID-19.
Fast forward three years, and the pandemic has now led to over 3 million cases in the state and nearly 29,000 deaths.
Meanwhile, local doctor’s offices across the state are still dealing with the changes, costs and damage the pandemic caused for the health care industry.
For example, at Oncology Specialists of Charlotte, masks are still required at the office every day.
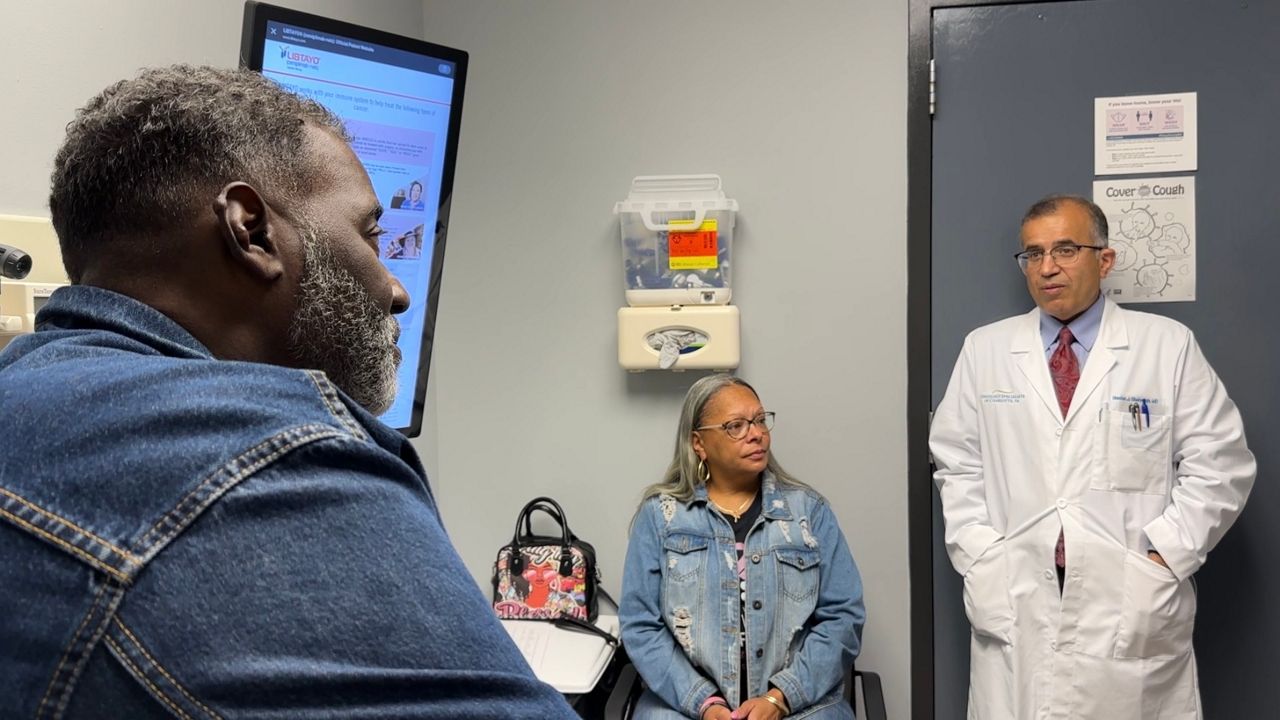
As Oncologist Justin Favaro gets up to speed on his patients for the workday, he says it is still a tricky business balancing the potential deadliness of cancer with the severity of COVID-19.
“If you have a low immune system to begin with, specifically lymphoma, leukemia, you can still get pretty sick from COVID. And so, we’re being very careful about those patients, making sure they still take precautions. And, if they do get COVID, treating them right away with medications,” Favaro said.
He says one of his patients experienced just that — and is still dealing with the consequences.
Michael Roy Land, who was first diagnosed with lymphoma in August 2014, says his recent health care struggles have been a journey.
“I come here every other week, getting chemotherapy. I’ve had a couple of relapses and they have to increase the dose, and then back down on the dose,” Land said.
Land added when he was first diagnosed, he was told there was a 20% chance he’d live five years.
The diagnosis was nearly nine years ago.
“I’m still here, so, their therapies work or I guess I’m one tough SOB, trying to keep God from taking me back home,” Land said with a grin.
But last May, it was not cancer that almost killed Land; it was COVID.
“It was near midnight. I wasn’t feeling well, felt like I had a cold. Took a home COVID test, and it was positive,” Land said, saying he had just returned from a trip to Europe.
Land says he continued testing positive for 13 more weeks, despite prescription drug treatment. Eventually, he developed breathing issues.
“Pulmonary interstitial pneumonitis, is a complication of COVID, and it’s very rarely seen before COVID. But now the doctors tell me it’s being seen because of people having had immunosuppression, having cancer, having chemotherapy, being diabetic, being rundown, and they said, ‘You fit all of those,’” Land recalled.
Land would know. He was a practicing physician for over three decades.
Meanwhile, Dr. Favaro says medical care and consultations have changed in several ways. There’s more emphasis on hygiene, and telehealth continues to grow in popularity for patients looking for basic sickness treatments, among other things. Favaro says both changes are likely to stay.
“I think [it] still gives us a lot of flexibility for patients and their schedules. The transportation costs are much higher, and I really hope that never goes away. I think that’s been a huge advantage for the care of the patient,” Favaro said, discussing the future of telehealth.
The pandemic has not just changed patient care. For some, it has also changed perspective.
“Before, I kind of ‘poo-poohed’ the whole thing. I thought the medical world was overdoing it. Now, I’m a very, very firm believer that COVID is alive, well and kicking. And, it’s definitely having some major impact on the world population. I’m very thankful I’m alive,” Land said.
Besides the changes to health care, COVID-19 has changed many lives across North Carolina. The North Carolina Department of Health and Human Services says North Carolina has had 3.4 million cases and 28,389 deaths.