WASHINGTON — The Biden administration is raising concerns about nearly 1 million Texas children dropped from the Medicaid program following the phaseout of pandemic-era coverage. Texas already led all states in the number of uninsured residents, even before the Medicaid rolls were reduced.
Graciela Camarena, outreach program director for Children’s Defense Fund-Texas, shared the shock of families in the Rio Grande Valley learning they lost or may lose health care under Medicaid, the health care program for low-income Americans.
“Some families saying, ‘Oh my God, you know, my daughter has this procedure already scheduled in October, I won’t have coverage, what’s going to happen, you know, she needs this.’ Families that said that they had scheduled surgeries or therapies,” Camarena said. “So it was very stressful for families.”
According to state data, Texas has removed more than 909,000 children from Medicaid since April following the end of pandemic-related protections. The data shows more than 715,000 lost coverage because of procedural problems, like not fully completing applications for new assistance once their pandemic coverage ended.
“It’s so important to be able to communicate, coordinate and assist families,” Camarena said. “Children’s Defense Fund is in the front lines. We’re talking to families and assisting and, you know, they trust us to bring to them this information. So we also need to make sure that process is going smoothly along the way.”
U.S. Health and Human Services Secretary Xavier Becerra wrote Gov. Greg Abbott, R-Texas, saying he was “deeply alarmed” by the removal of hundreds of thousands of Texas children from the Medicaid rolls.
“We are urging our colleagues at the state level, including in Texas, to take up more of those options, all of which have the effect of keeping eligible people connected to health care coverage and also reducing the amount of red tape and headache people have to go through just to renew benefits that they’re still eligible for,” said Daniel Tsai, the deputy administrator and director of Center for Medicaid and CHIP services.
Among those options Biden administration officials are asking Gov. Abbott to consider is using state funds to expand Medicaid, which Texas has refused to do.
“Expanding Medicaid will help many people including an 18-year-old kid that turned 19, who falls into a coverage gap because there is no Medicaid expansion and they have no other coverage option, and that policy choice will have a huge impact on people’s ability to access what we believe is a human right,” Tsai said.
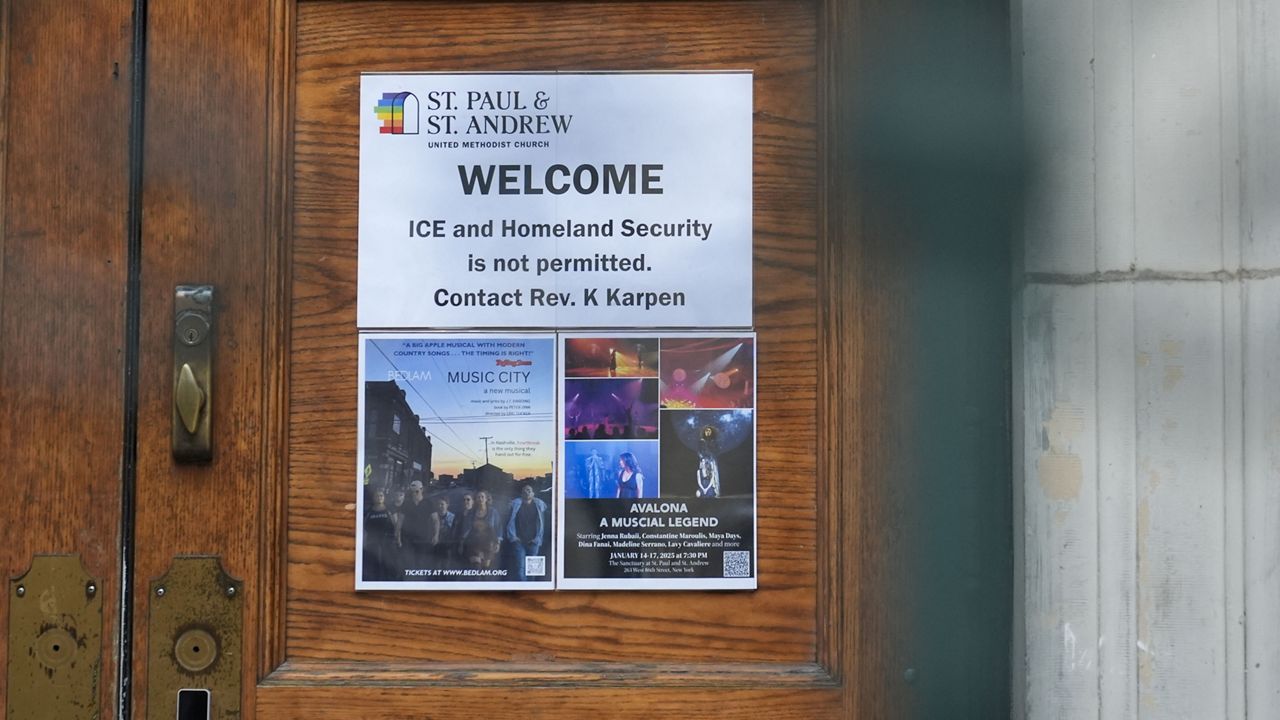
In a statement to Spectrum News, state health officials said in part that redetermining eligibility is a “massive undertaking” and they meet regularly with federal partners to ensure the process is successful and follows the law. The spokesperson said that the Texas Health & Human Services Commission is “committed to ensuring that those qualified for benefits receive them.”