CHAPEL HILL, N.C. — Representatives from Pfizer revealed their intent to submit an application for a vaccine targeting a contagious respiratory illness in children to the Food and Drug Administration by the end of this year.
All 20 beds in the UNC Children's Hospital PICU are full
Parents seeking care for their sick children are being redirected to other health systems
Critical care is slammed due mainly to respiratory illness
Scientists at the pharmaceutical company gave pregnant mothers participating in a study a shot against respiratory syncytial virus in hopes of passing antibodies on to their children.
This potential breakthrough would be intended to give newborns greater protection after birth.
While this could become the first RSV vaccine, the immunization can’t reach children already sick with the illness in critical care across North Carolina.
Respiratory sickness is filling up hospitals across the state, including the UNC Children’s Hospital.
A spokesperson confirms all 20 of the beds in their Pediatric Intensive Care Unit are full.
The sight of nurses rushing into a patient’s room can happen at any time on the floor.
“I think it has been extremely challenging, and I think it has been an extremely busy time,” Dr. Benny Joyner said.
Joyner hardly has time for a break.
“As soon as we are able to get to a point where we can get patients discharged, patients treated and able to go home, it turns right around and there are more coming in,” he said.“As soon as we are able to get to a point where we can get patients discharged, patients treated and able to go home, it turns right around and there are more coming in,” he said.
Much like health care teams across the country, the UNC health system is at max capacity mainly because of a rise in respiratory illnesses like RSV. At last check, two-thirds of all cases at UNC Hospitals in Chapel Hill belonged to people under the age of 18.
Joyner, the chief medical officer of the PICU, said at one point over the last week, there were 10 or more patients waiting in the emergency department for a bed.
“... Who are waiting in the E.D. (emergency department) on those stretchers for six, eight, 10, 12, up to 18-24 hours,” he said.
There is no available space in critical care.
“If we don’t have any beds available in the ICU, and we don’t have any beds available on the floors, then we are not going to be able to take any patients into the hospital,” he said.
Joyner said they are not only treating sick children in the Triangle — but across the state – as UNC Children’s is also a referral hospital.
Some rural areas don’t have pediatric treatment facilities anymore because those medical centers have been shut down.
“For me specifically, here in the ICU, part of the reason I went into the intensive care world is because I am the stop for the sickest of the sick. Whenever there’s a call for assistance I want to try to be there to help. To say that unfortunately we don’t have any more beds to put you in so we can’t safely treat you is really a heartbreaking thing,” he said.
Joyner said at least 75% of patients receiving long-term critical care are being seen for some sort of respiratory ailment. It’s impossible to move patients in when you are not moving them out.
The dilemma creates a moral conflict for the head of the critical care unit.
“I don’t know if I can appropriately describe the challenge, because it is a significant moral injury. The reason we get into this is we try to help children,” he said.
According to multiple pieces of medical literature, a moral injury can occur when a health professional must follow a rule which goes against their core values. One example is how safety protocols did not allow people to be at the bedside of a dying family member at the height of the pandemic. Sometimes nurses, doctors and other staff were forced to watch those patients die from COVID-19 alone when there was nothing else they could do.
Joyner said recently when there have been as much as 80-90% of ER patients awaiting care in the PICU, the call was made to reroute families seeking care to other hospitals or medical systems.
The inability to change circumstances creates anxious days and nights for the UNC PICU team.
It’s a theme playing out during this pandemic when COVID-19 protocols kept nurses from providing the same care they did outside the public health crisis.
“One of the issues for us we alluded to is the increase of nursing turnover,” he said.
It’s why Joyner checks on staff regularly.
That demand grows harder to meet with nurses leaving the profession in droves. As many as 90% who responded to one survey have considered leaving the business over the last year.
He called the bedside and respiratory nurses the glue holding the floor together.
“Every day we are trying to make sure that we not only have a stock of resources and physical support, but the supplies that we need,” he said.
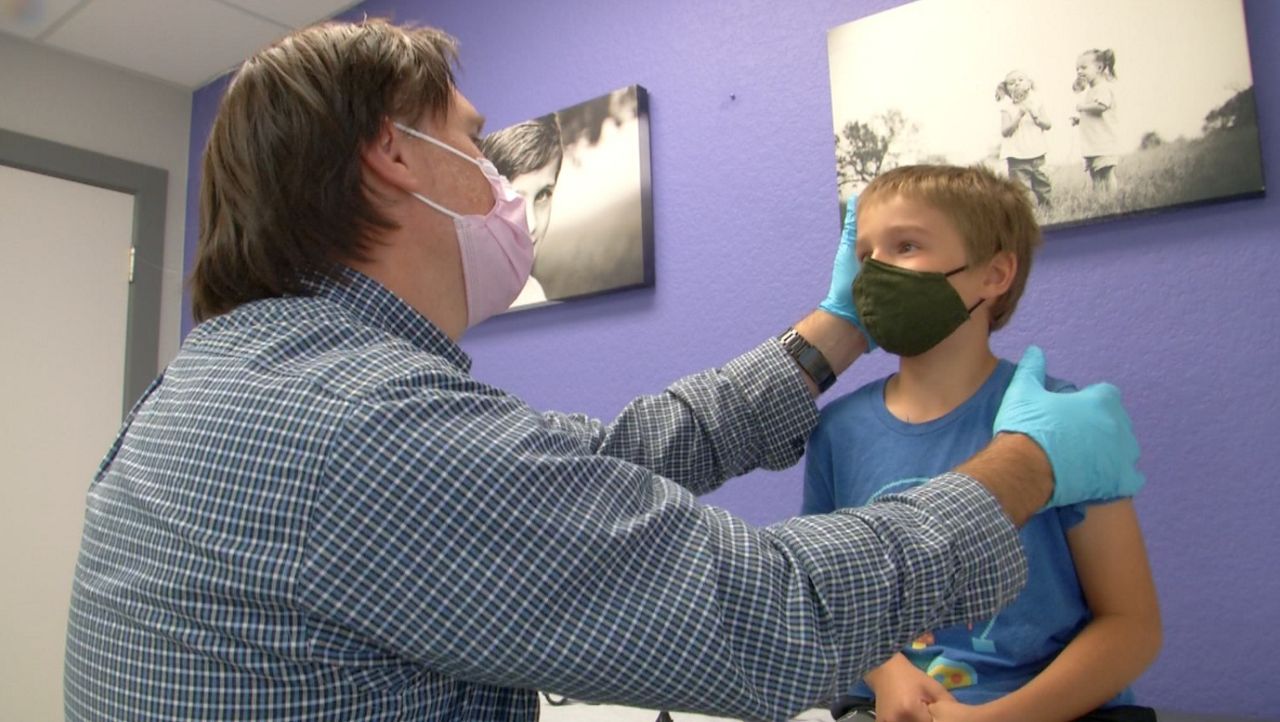
One cause for a spike in respiratory illnesses for children has been the removal of masks, relaxation of social health guidelines and an exposure to viruses younger bodies may not be used to at this point in life.
“We’ve probably noticed this ever since the masks came off last year that kids started to go back and started to socialize and started to engage as all kids do. We started to see the recurrence of respiratory illnesses,” he said.
The high emotional burden of providing constant care is why the doctor walks the floor as often as he can.
“Welcome back,” he said to one staff member who worked her first shift since going on maternity leave.
Infants, toddlers and children with chronic medical conditions have been hit hard.
Amid all the monitors, buzzing and beeping, are real people trying to make this place a home for sick children. Art is drawn on almost all the glass windows to each child’s room. Some designs included familiar characters from familiar stories like Piglet and Pooh.
However, when the space they work in cannot provide all the care these patients need it leads to heartbreak, for even Joyner.
“It is extraordinarily challenging to hear a colleague on the other line calling you to say, ‘I would like to transfer this kid up here. This child is extremely ill and needs your services at UNC.' And for us to say, ‘I hear you and I want to help but I can’t do it,’” he said.
Joyner says these are RSV symptoms:
- Runny nose
- Decrease in appetite
- Coughing
- Sneezing
- Fever
- Wheezing
The Centers for Disease Control and Prevention listed no specific treatment for RSV infection. There is, however, medical guidance on what parents should do if their child exhibits more serious symptoms like labored breathing.