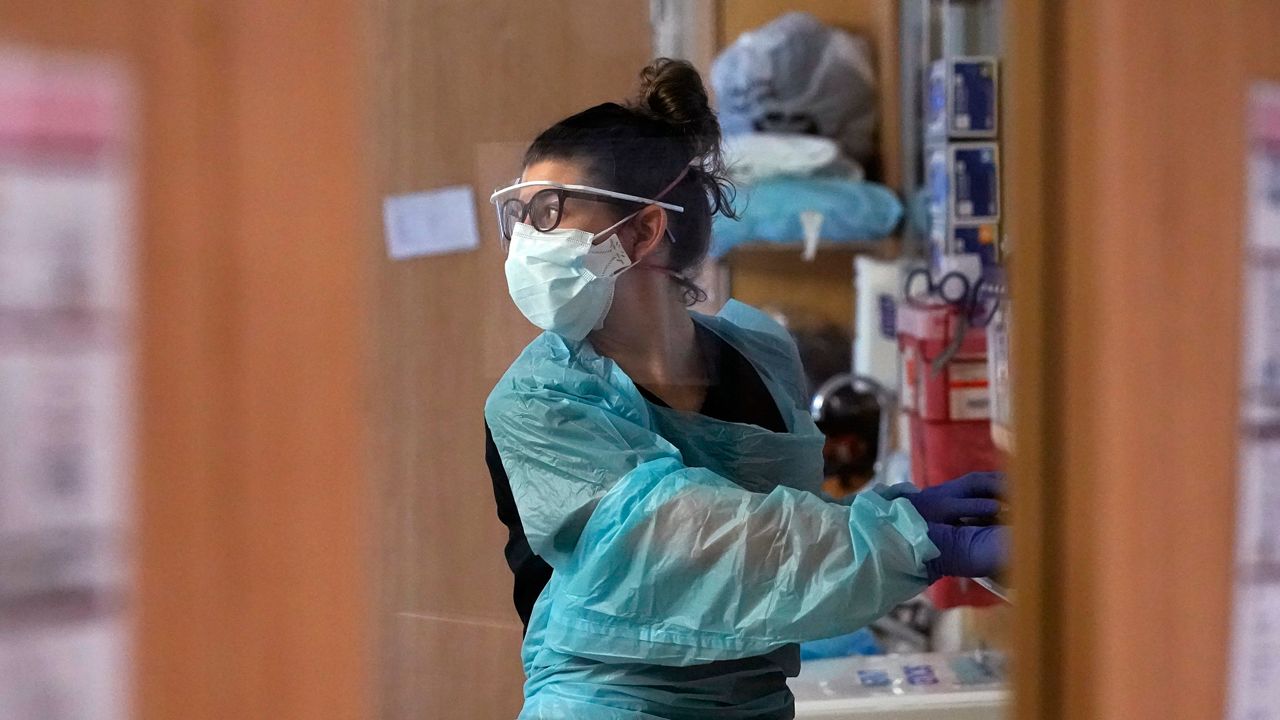
Hospital officials told lawmakers Friday they are struggling to keep up with the demands of the pandemic, even with COVID-19 hospitalizations declining.
At Eastern Maine Medical Center, they set a new record this week with 60 people waiting in the emergency department needing help for behavioral health issues, said Lisa Harvey-McPherson, vice president of government relations for Northern Light Health.
EMCC also had a pandemic-high 618 employees out because of COVID across their facilities.
In addition, EMCC set a record with more than 120 patients needing to be transferred to nursing homes with no place to go, she said. Many nursing homes can’t take new patients because their staffing levels are down 28% since the start of the pandemic.
“The staffing challenge is the No. 1 reason we are not able to discharge acute care patients into a long-term care bed,” Harvey-McPherson said. “But we also have ongoing COVID-19 outbreaks in our nursing facilities.”
Harvey-McPherson was one of three hospital representatives to address members of the Legislature’s Health and Human Services Committee on Friday. Committee chairwoman Rep. Michele Meyer (D-Eliot) said she invited them to speak because “our hospitals are under intense pressure.”
At MaineHealth facilities in southern Maine, they are “busting at the seams” despite doubling the number of intensive care beds at Maine Medical Center and adding 94 additional beds throughout the system, said Katie Fullam Harris, chief government affairs officer. To address the COVID surge, they have delayed 2,138 non-emergency surgeries.
“That backlog of surgical cases is really troubling,” Fullam Harris said. “Some of those cases are cancer patients. These are surgeries that are necessary and they are going to result in some real challenges for us over the next few months and probably a year.”
When it comes to the emergency department, Fullam Harris said use at Maine Medical Center is “through the roof.”
Another layer of stress comes from the closure of group homes that serve people with intellectual disabilities or mental health challenges. The Maine Medical Center emergency department has had one person with intellectual disabilities spend four months waiting for a place to live and another there for 54 days, she said.
“We just can’t have emergency departments as the place of last resort for people who need specialized residential treatment,” Fullam Harris said.
In November and December, 85 children spent between two and 20 days waiting in the emergency department, she said, a problem made worse by the pandemic, but not created by it.
When it comes to staffing, MaineHealth has added 1,000 jobs to meet demand but has struggled to hire enough staff. In January of last year, they had 1,323 positions open and this January they have 2,700 jobs open. Of those, 847 are nursing positions.
Fullam Harris said burnout has been a factor challenging health care workers.
“It’s been hard getting yelled at by patients, getting yelled at by families who are frustrated because we’ve had to implement policies and procedures related to visitation,” she said.
MaineHealth on Friday instituted new return-to-work guidelines for health care workers that allow them to come back following a COVID infection if they are fever-free for 24 hours. They do not need to take a COVID test to return to work, she said.
The vaccine mandate for health care workers resulted in the loss of 3% of the workforce at Northern Light facilities and 2% at MaineHealth facilities, the spokeswomen said.
Maine Hospital Association Vice-President Jeff Austin said hospitals across the state are facing an array of financial challenges. First, he said hospitals delayed surgeries in the spring of 2020 “at the governor’s request” to prepare for a wave of COVID-19 cases that never materialized.
Second, costs are up significantly for pharmaceuticals, personnel and personal protective equipment, he said. And third, because they’ve had to delay surgical services again in response to the omicron wave, they are bringing in less revenue.
“The service mix has changed and that’s carried a cost to our bottom line,” he said.
With that in mind, the hospital association has asked Gov. Janet Mills to provide them with additional funding in her supplemental budget that’s due to be released in the coming weeks. That includes an $8 million one-time payment, reducing the impact of a hospital tax and assistance with building out infrastructure needed for the continuation of telehealth services.
Sen. Joe Baldacci (D-Bangor) said he hopes the committee can work to help get some additional funding for hospitals.
“I am very concerned about what you have presented today,” he said. “It’s clear these trends are not sustainable and that unless there’s relief in general it’s going to threaten the lives of more people, not just with COVID, but people looking for other types of surgeries.”