OHIO — While there is no treatment for neurodegenerative conditions, including Alzheimer’s Disease, a new drug has been identified that could help treat the conditions by investigators at Case Western Reserve University, University Hospitals and Louis Stokes Cleveland VA Medical Center.
Across the globe, more than 55 million people have dementia caused by Alzheimer’s Disease (AD) and other conditions that destroy cells in both the brain and nervous system.
Through collaborative efforts, the drug and the approach used with it have shown promising results in mouse models of AD. The study was published in the Proceedings of the National Academy of Sciences.
“Our findings suggest an effective new way to safely prevent neurodegeneration and cognitive impairment in Alzheimer’s disease by directly protecting the blood-brain barrier (BBB),” said the study’s co-lead researcher Andrew Pieper, a psychiatrist and neuroscientist at the Case Western Reserve School of Medicine and the Morley-Mather Chair of Neuropsychiatry at University Hospitals Cleveland Medical Center.
Pieper said in mouse models treated with the drug, the blood-brain barrier remained undamaged.
“The brains didn’t undergo neurodegeneration and, most importantly, cognition and memory capacity were completely preserved,” he said.
Co-leading the study was Sanford Markowitz, the Ingalls Professor of Cancer Genetics and Distinguished University Professor at the Case Comprehensive Cancer Center and Division of Hematology-Oncology Department of Medicine at Case Western Reserve and University Hospitals.
Through the study, scientists targeted the blood-brain barrier, which is a network of cells that form a layer between the brain and the blood rather than neurons in the brain.
Researchers said the deterioration of the barrier is an early indicator of many forms of neurodegenerative diseases, including AD.
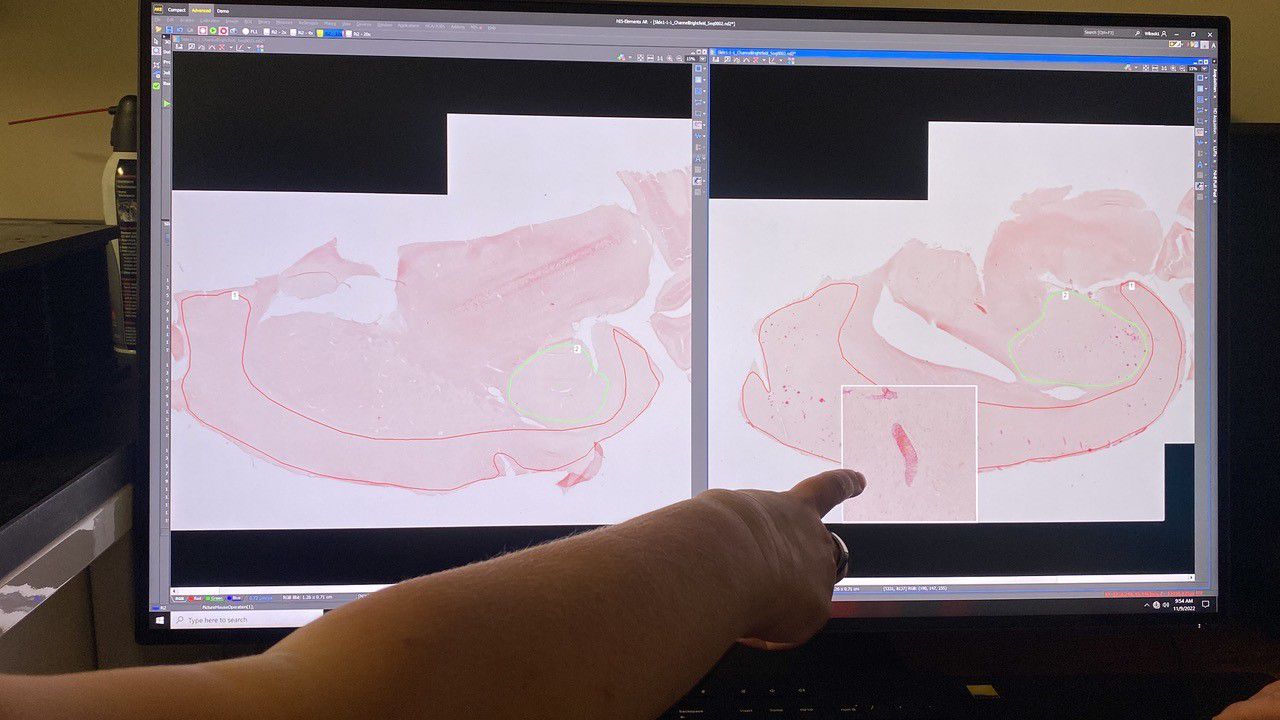
They specifically targeted an enzyme known as 15-PGDH, or 15-hydroxyprostaglandin dehydrogenase, which is highly enriched within the blood-barrier. Through the study, they discovered the enzyme is elevated in AD, traumatic brain injury and aging in both mice and humans, which harms the blood-brain barrier.
The team developed a drug, SW033291, at Case Western Reserve School of Medicine and University Hospitals to block the enzyme.
It was originally developed in the Markowitz lab for a different purpose, to activate stem cells to repair tissue damage in mouse models of colitis and bone-marrow transplants.
“Finding together that blocking 15-PGDH also blocks brain inflammation and protects the BBB was an exciting new discovery,” Markowitz said. “Notably, SW033291 didn’t change how much amyloid—a sticky protein that accumulates in Alzheimer’s—was in the brain. This is important because the most recently approved AD drugs focus only on removing amyloid and, unfortunately, don’t work very well and have risky side effects. Inhibiting 15-PGDH thus offers a completely new approach for AD treatment.”
Through the study, researchers saw by using the drug to inhibit the enzyme, the mice were protected from neurodegeneration and cognitive impairment after a traumatic brain injury, such as a concussion. The results showed even when the drug was administered a day after the injury.
Scientists hope the drug can help treat AD, brain injuries and other brain diseases.